Psoriasis is a common inflammatory skin disorder that affects both children and adults. It is characterised by thick, red, scaly plaques that can be localised or devastatingly widespread.
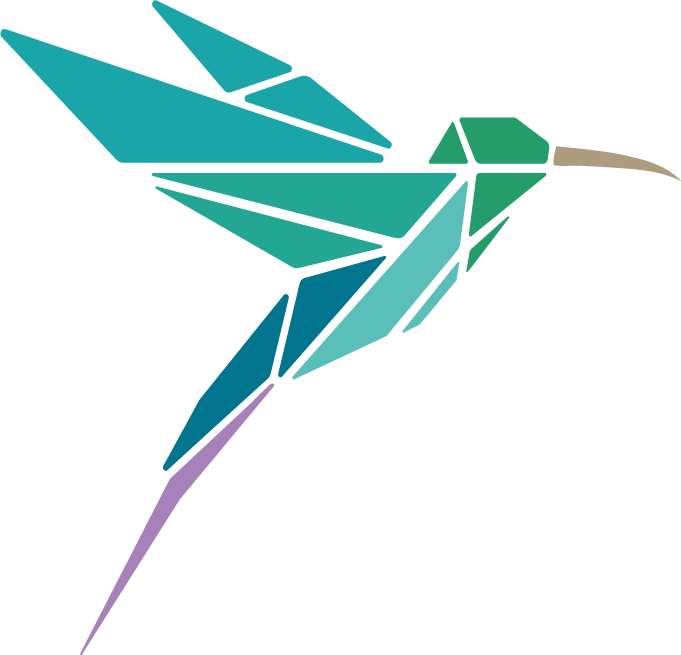
Psoriasis can start at any age and is caused by a complex interplay of genetic, environmental and immunologic factors.
It is a chronic, ie lifelong, condition with fluctuating severity over time.
Psoriasis sufferers often have associated systemic diseases such as obesity, depression and inflammatory bowel disease.
Depression is one of the important factors that impairs the quality of life of people with psoriasis. Psoriasis can lead to depression, and depression, in turn, exacerbates psoriasis.
Although there are many contributing factors in this complex disease, recent research has shown that there may be one common denominator- your gut health.
![]() The gut-brain-skin axis and psoriasis
The gut-brain-skin axis and psoriasis
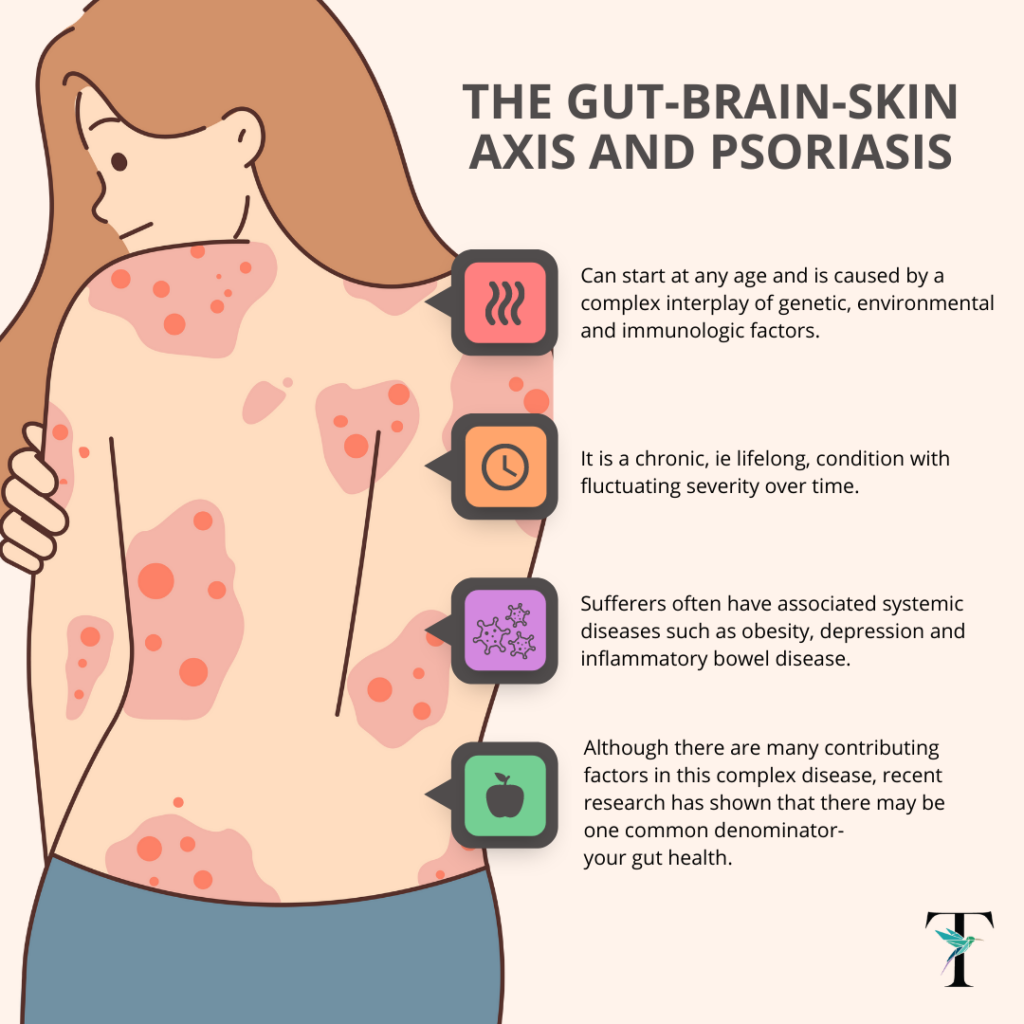
The gut-brain-skin axis has been used to explain correlations among the gut microbiome, emotional states and systemic and skin inflammation.
As early as 1930, dermatologists John Stokes and Donald Pillsbury suggested that emotional states such as anxiety and depression can alter the gut microbiota and induce local or systemic inflammation. They recommended the use of fermented milk to reintroduce beneficial microorganisms.

Stress leads to the release of neurotransmitters (like serotonin and norepinephrine). These neurotransmitters increase gut permeability, leading to local inflammation. At the same time they also provoke systemic inflammation via the bloodstream.
For example, the stress hormone cortisol is thought to alter the composition of the gut microbiota and blood levels of neuro-endocrine molecules, ultimately affecting the skin barrier and skin inflammation.
The gut-brain-skin axis is bidirectional, ie the skin can in turn act on the gut via the nervous system.
Gut dysbiosis (the imbalance of gut microbiota) makes the gut barrier more permeable to pro-inflammatory cells, which via the blood stream are thought to play a role in skin dysbiosis (the imbalance of skin microbiota). In addition gut dysbiosis may modify the production of neurotransmitters, also affecting skin function.
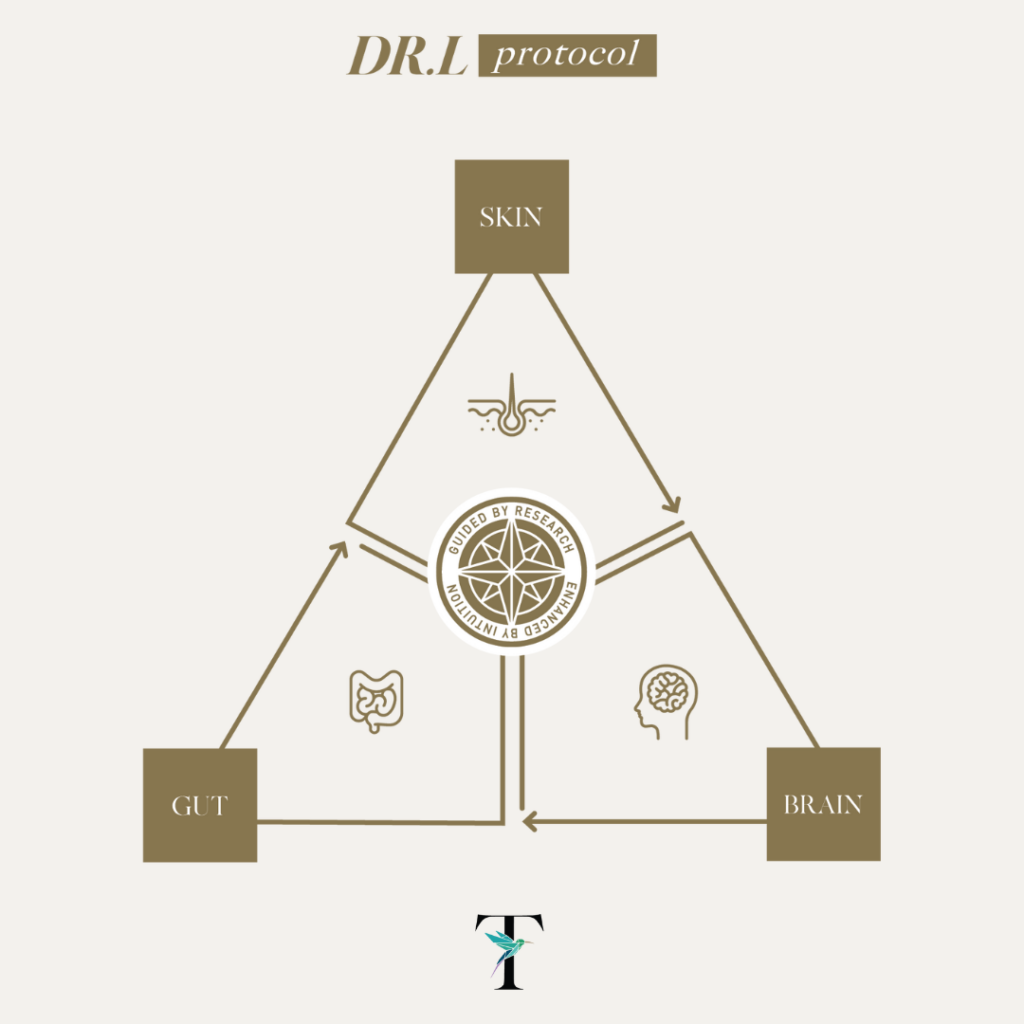
There is a close association between psoriasis and dysbiosis of both gut and skin microbiota.
Several studies have shown that the gut microbiota of psoriasis patients displayed a lower diversity and relative abundance of certain bacteria. Accumulating evidence also suggests an abnormal composition of skin microbiota in psoriasis patients.
Psoriasis is tricky to treat as although traditional therapies are effective, they have several side effects.
Interventions that modulate the microbiota- including probiotics (oral and topical) and faecal microbiota transplantation bring hope to psoriasis sufferers.